- Spotting
- Posts
- The Hidden Reason Women Feel Wiped Out
The Hidden Reason Women Feel Wiped Out
Doctors think you’re fine. Your iron disagrees.
If you're a Rescripted fan, you know we love spotlighting people who see gaps in care firsthand — and then do something about them.
Enter Elise. She’s our Director of Partner Content, and a tireless patient advocate in the rare disease community since 2010. Over the years, she’s worked on issues from Dystonia to Lyme disease to Ehler-Danlos syndrome, even helping drive multiple bills in Congress to improve research funding and care.
I work closely with Elise, and when she told me about her iron infusion experience, I was equal parts frustrated and impressed — frustrated that the system failed her, and impressed by how fiercely she advocated for herself. I convinced her to share her story about ferritin today in Spotting.
Here’s Elise:
💌 But first: Can’t find Spotting in your inbox? Check Promotions (or Spam, grrr), drag us back, then add [email protected] to your contacts and ⭐ us, so we always land right where we belong 🤗
This Week’s Signal
Ferritin is quietly showing up as a key women’s health marker — one that many women are already symptomatic from long before their labs say anything is wrong.
As someone with a laundry list of rare diseases, the thing that’s taken me out the most lately wasn’t rare at all — it was my iron. Or more accurately, the lack of iron storage in my body.
About a month ago, after a couple of hospital visits for an unrelated issue, I followed up with my PCP for bloodwork because I still felt off. Even with heart conditions and rare diseases, I’d been working out twice a week and walking long distances every day. But over the past few months, I was exhausted, short of breath, and, at my lowest, could barely stand to make dinner or drive more than ten minutes.
When the bloodwork came back, my ferritin was low. My PCP said it was fine and to keep taking oral iron supplements (which I already had been). I wanted another opinion, so I reached out to my cardiologist: “Hey, my ferritin is <15. What do you recommend?” Their answer: “An iron infusion, ASAP.”
Even with iron supplements and my intuitive eating habits (I’d been having iron-fortified cereal and a green juice packed with vitamin C every morning), my body wasn’t keeping up. It had been trying to course-correct, but diet and supplementation alone weren’t enough. And sure enough, the infusion made all the difference.
Turns out, when your iron stores are depleted and you have heart problems, it can make them a lot worse. And so began my crash course in ferritin.

In addition to being our Director of Partner Content, Elise is also our resident Meme Qween 👑
What We’re Missing
If ferritin isn’t something you monitor like a hawk on your bloodwork, you’re not alone. Most of us aren’t taught to — and the gap between lab reference ranges and how women actually feel is enormous.
Ferritin measures how much iron your body has stored. Even if your iron levels look normal, low ferritin can still mean major issues. Yet most labs list ranges as low as 4-10 ng/mL. Meaning: if you’re above that, you’re “normal.”
Which led me to the question: Why does the lab say I’m okay when I am clearly not okay?
Hematologists, iron researchers, and the World Health Organization have been clear for years that women can experience symptoms well above those cutoffs — often below 15-30 ng/mL.
Iron deficiency, even without full-blown anemia, causes fatigue, brain fog, shortness of breath, exercise intolerance, mood changes, and autonomic symptoms. In fact, many women experience symptoms when ferritin dips below 75 ng/mL — far higher than the lab “normal” range.
When I started reading the research, I felt both validated and indignant — and I quickly realized that this gap is a subtle (and exhausting) form of medical gaslighting.
What We’re Seeing
The science, the guidelines, and women’s lived experiences are finally starting to line up — even if the system hasn’t fully caught up yet.
The American Medical Association estimates that nearly one-third of American women are iron deficient. The World Health Organization has been flagging iron deficiency for years as one of the most common nutrient deficiencies worldwide, disproportionately affecting menstruating women. And as I write this, the American Society of Hematology is actively reviewing proposed guideline updates that would raise the ferritin threshold for deficiency from under 15 ng/mL to under 30 ng/mL.
Translation: the bar is moving — slowly, but meaningfully.
At the same time, patient communities are far ahead of the guidelines. Spend five minutes in forums like r/Anemia and you’ll see story after story that looks eerily familiar: women dismissed for years, told their labs were “fine,” only to experience dramatic improvement once iron stores were actually addressed — often through infusions when supplements didn’t cut it.
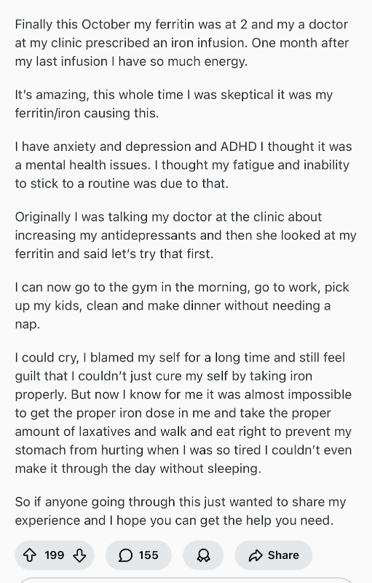
Exhibit A!
I lived this myself. I walked into my first iron infusion fully prepared to wait weeks for results. My infusion was at 2pm. I went home assuming I’d crash. Instead, that night, I walked my dog, decorated my tree, and baked three dozen cookies. I didn’t feel magically cured — but the fog lifted, the color came back to my face, and for the first time in months, I felt like myself again.
That was the moment I realized just how much I’d normalized feeling unwell — and how common that normalization is for women.
What It Means
Ferritin isn’t just a lab value. It’s a missing conversation in women’s health.
We spend (rightful) time talking about hormones — cortisol, thyroid health, burnout, gut health. But iron is foundational. It impacts oxygen delivery, energy production, neurological function, heart rate regulation, even mental health. In other words: every system that helps you be a functioning human.
When ferritin is low, everything feels harder. And yet, many women are told they’re “fine” because their labs technically fall within range. That disconnect isn’t benign — it delays care, erodes trust, and leaves women questioning their own bodies.
This is where awareness and self-advocacy matter. If your labs say “normal” but your body says “absolutely not,” that tension is worth investigating. Ask questions. Bring research. Ask your provider to look again. Bring a trusted friend if you need backup.
There’s a real chance it’s not just anxiety, burnout, or hormones. Your body might also be begging for iron.
For me, understanding ferritin changed everything — and I’m eagerly awaiting my next infusion as my iron stores rebuild. But zooming out, this feels bigger than my story. If we start treating ferritin as a functional health marker — not just a checkbox on a lab report — it could be one of the next major shifts in women’s health.
It shouldn’t be this hard to feel okay. Talking about ferritin is a place to start.
Elise said it best: this is solvable. Low ferritin isn’t just a number — it’s a functional marker showing your body’s iron stores are depleted, which can impact energy, cardiovascular function, and neurological health. With the right care, those effects can be reversed, and women can reclaim the vitality they deserve.
Lab reference ranges evolve slowly, but our understanding of women’s health is advancing rapidly. Paying attention to overlooked markers like ferritin is a way to advocate for your body with evidence, not guesswork.
Huge thanks to Elise for sharing her story and shining a light on a lab value too often dismissed. If her experience has you thinking about your own ferritin, you’re not alone — and it’s worth a conversation with your provider.
With more signal and less noise, Spotting is your weekly lens on what’s next in women’s health — and why it matters. See you right here next time, in your inbox. (And if a friend forwarded this to you, you can subscribe to get your own copy.)
With hugs, science & freedom,
Abby
P.S. Whether this hits or misses for you, I’d love to hear your thoughts — just hit reply. Thanks for being here 🤗

Reaching 20M women monthly and partnering with trusted brands like Pfizer, Kotex, BetterHelp, and Noom, Rescripted is the leading media platform for all women and their health, from first period to last period.